Lyme Disease and Mental Health: Personality Shifts Explained
When most people think of Lyme disease, they imagine fever, fatigue, and joint pain. But there's a lesser-known side to this illness—its deep impact on mental health. The relationship between Lyme disease and mental health is complex, often leading to unexpected changes in mood, behavior, and even personality.
For many, the emotional and psychological symptoms of Lyme disease can be as debilitating as the physical ones. In this blog, we’ll explore how Lyme disease affects mental health, the signs of personality shifts, and ways to manage these changes with compassion and care.
What Is Lyme Disease?
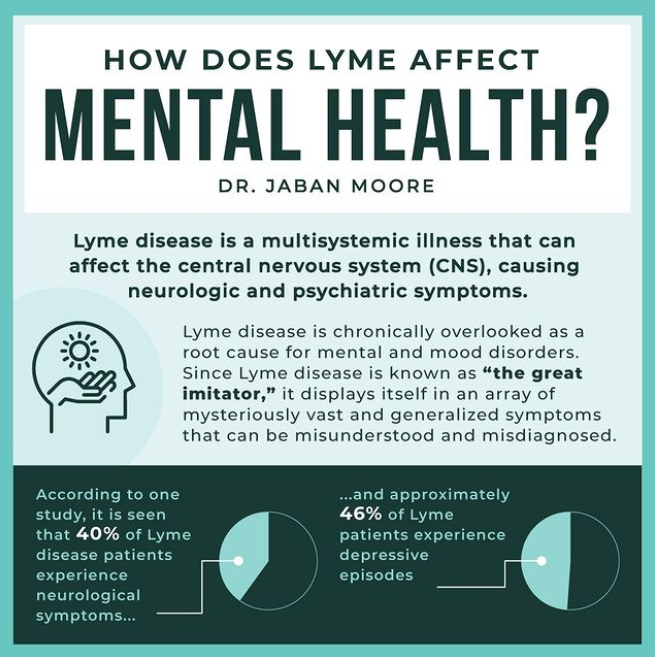
Lyme disease is an infectious illness caused by the bacterium Borrelia burgdorferi, transmitted through the bite of infected black-legged ticks. When detected early, it’s often treatable with antibiotics. However, if left untreated or not fully eradicated, Lyme disease can spread to the nervous system and brain—leading to neurological and psychiatric symptoms.
This neurological form of Lyme is often referred to as neuroborreliosis and is at the heart of many mental health-related symptoms.
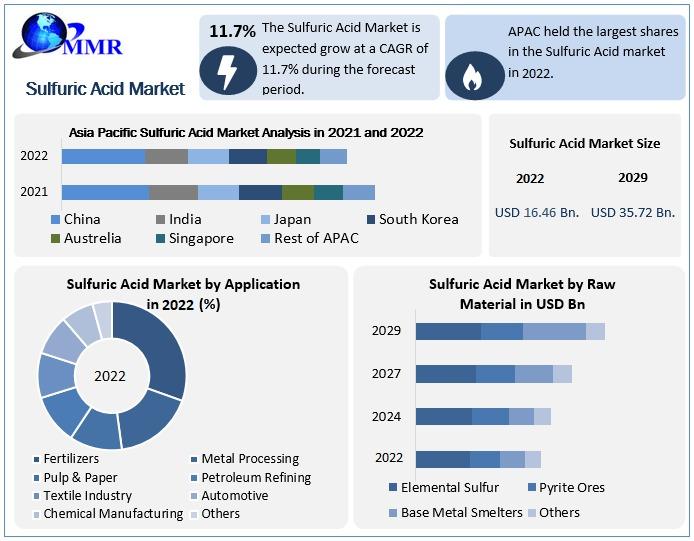
The Link Between Lyme Disease and Mental Health
The brain and immune system are intricately connected. When Lyme bacteria invade the central nervous system, they can cause inflammation in the brain and disrupt normal brain function. This inflammation can affect neurotransmitters, such as serotonin and dopamine, which regulate mood and cognition.
As a result, people with Lyme may experience a wide range of mental health symptoms, even if their initial infection seemed mild. These may include:
-
Anxiety
-
Depression
-
Panic attacks
-
Insomnia
-
Brain fog
-
Personality changes
-
Mood swings
For some, these symptoms can persist even after the infection is treated—this is often referred to as Post-Treatment Lyme Disease Syndrome (PTLDS).
Common Mental and Emotional Symptoms of Lyme Disease
1. Personality Changes
People with chronic or late-stage Lyme disease often report feeling "like a different person." Loved ones may notice sudden shifts in behavior, including:
-
Increased irritability
-
Emotional outbursts
-
Withdrawal from social settings
-
Apathy or lack of motivation
-
Increased sensitivity or suspicion
These changes can be distressing and often misunderstood, especially when there’s no visible sign of illness.
2. Anxiety and Panic
Anxiety is a common symptom of Lyme disease. It may manifest as general unease, obsessive thoughts, or sudden panic attacks. This can occur even in individuals with no history of anxiety disorders.
3. Depression
Due to both neurological and lifestyle impacts (loss of work, isolation, chronic pain), depression frequently occurs in those suffering from Lyme disease. Some people experience deep sadness, hopelessness, or suicidal thoughts and should seek professional help immediately.
4. Cognitive Impairments ("Brain Fog")
Memory problems, difficulty concentrating, and confusion are common complaints. This mental fatigue can interfere with daily activities and contribute to emotional distress.
Why Are These Symptoms Often Misdiagnosed?
One of the biggest challenges with Lyme disease and mental health is misdiagnosis. Because the symptoms overlap with those of psychiatric disorders, many individuals are mistakenly diagnosed with:
-
Depression
-
Bipolar disorder
-
Generalized anxiety disorder
-
ADHD
-
PTSD
Without proper testing and awareness, the root cause—Lyme infection—may go undetected for years. That’s why it’s crucial to consider a patient’s full medical and environmental history, especially if they’ve been exposed to tick-prone areas.
Managing Mental Health Challenges in Lyme Disease
There is no one-size-fits-all solution for mental health symptoms related to Lyme disease. Treatment must be multidimensional, combining medical, psychological, and lifestyle support.
1. Medical Treatment
-
Antibiotics: To target any remaining infection.
-
Anti-inflammatory therapies: To reduce brain inflammation.
-
Supplements: Including B vitamins, omega-3s, and herbal support (consult with a healthcare provider).
2. Mental Health Care
-
Therapy: Cognitive Behavioral Therapy (CBT) and trauma-informed care can be beneficial.
-
Medication: In some cases, antidepressants or anti-anxiety medications may provide relief.
-
Mindfulness practices: Such as meditation and yoga can help regulate emotions.
3. Holistic and Lifestyle Support
-
Nutrition: An anti-inflammatory diet supports both brain and immune function.
-
Exercise: Gentle movement like walking or stretching can improve mood.
-
Sleep hygiene: Proper rest is critical for emotional and physical recovery.
-
Support networks: Joining Lyme disease support groups—online or in person—can help patients feel less isolated.
Supporting a Loved One with Lyme-Related Mental Health Issues
Watching someone change because of Lyme disease can be painful and confusing. It’s important to remember that these shifts are not intentional—they are symptoms of a serious illness. Here’s how you can help:
-
Be patient and nonjudgmental
-
Encourage them to seek professional help
-
Educate yourself about Lyme disease and its mental health impacts
-
Offer emotional support and validation
-
Help track symptoms for doctor visits
Empathy and understanding go a long way in supporting healing and rebuilding relationships strained by the disease.
Final Thoughts
The connection between Lyme disease and mental health is real, complex, and often overlooked. From anxiety and depression to noticeable personality changes, the emotional impact of Lyme can be just as severe as the physical toll.
If you or someone you know is struggling with unexplained mood changes and has been exposed to tick environments, Lyme disease should be considered as a possible cause. With the right care, many people do find relief and recovery.